PDF Version
TO: All Providers
Effective 5/6/2020, claims which have other
commercial insurance primary (not Medicare) that have denied the services can
be submitted electronically. The list of denial codes that may be submitted
electronically can be found here:
https://medicaid.alabama.gov/content/7.0_Providers/7.1_Third_Party.aspx. Providers will
complete a simple form, attach TPL Explanation of Benefits and upload
electronically. Once the form has been completed an electronic claim can then
be submitted for review.
First, upload supporting documentation and
receive an ACN (Attachment Control Number) to be used in claims submission.
Please follow these steps:
Accessing the
Medicaid Interactive Web Portal
A secure logon to the Medicaid Interactive
Web Portal is required to access the new TPL Claims Form. TPL Claims supporting
documentation may be submitted in two different ways:
•
Medicaid Interactive Web portal (preferred)
https://www.medicaid.alabamaservices.org/ALPortal/.
• Fax information using barcode cover sheet received
after submitting the form in the web portal.
Browser
Compatibility
Follow the below instructions to set their browser
compatibility settings:
•
Navigate to the Medicaid Interactive Web
Portal using the URL provided above.
•
Select Tools
from upper right-hand corner of browser. The feature is displayed as a wheel.
•
Choose Compatibility
View Settings.
•
Click Add.
•
Click Close.
• Refresh Browser to apply setting.
Documents must be
in a Portable Document Format (PDF)
Documents must be in a PDF for upload
through the Web Portal. If you do not currently have the ability to create PDF
versions of supporting documentation, you may perform an internet search and
find free downloadable utilities that can be installed to create a PDF. For
your convenience, DXC is including a list of three PDF creation utilities that
can be installed to create PDF documents at no charge:
•
PrimoPDF - http://www.primopdf.com/
•
Solid PDF Creator -
http://www.freepdfcreator.org/
• PDF24 - http://pdf24-pdf-creator.en.softonic.com/
Steps to Upload
Documentation
Once a PDF utility
has been successfully downloaded and the PDF document created, providers should
follow these steps to upload documentation for review:
- Log on to Medical Interactive Web portal by
going to the following link and selecting Secure Site: https://www.medicaid.alabamaservices.org/ALPortal/.
- Select
Trade Files/Forms.
- Select the “TPL Claims Attachment Supporting Doco”
form from the drop-down list and click on Search.
- Complete all fields on the form (Record ID and
Attachment Control Number fields will auto populate). Required fields are
indicated with an asterisk (*).
- Click Browse
and select the required TPL Explanation of Benefits documentation from
your network drive or PC.
- Review all the values entered for completion
and accuracy as no further updates will be allowed once the Submit button
is pressed. Note: If any error
messages are presented, resolution of the identified errors is required to
complete submission.
- Press Submit.
- A message will be generated at the top of the
page that states “Your form was submitted successfully."
- A barcode cover sheet is generated and will be
displayed. It is imperative that
you save a copy of this cover sheet should you be requested to submit
additional documentation for this packet.
- Select the Print Friendly
View button to print the barcode cover sheet.
Steps to FAX Documentation
Information can also be faxed in for review.
Providers should follow the instructions below to fax documentation:
- Follow steps 1-10 documented above.
- Include the barcode cover sheet as page one of
the fax transmission for the corresponding attachment control number.
- Fax the required documentation with the
barcode cover sheet on top to (334) 215-7416. Important: Barcode cover sheets are unique to each TPL Claims form
submission. DO NOT use it for
another TPL Claims form submission.
- DO NOT place anything over the barcode on the cover sheet or alter it in
any manner.
- DO NOT fax double sided pages.
- DO NOT fax multiple sets of records at the same
time, each fax should be sent separately.
NOTE:
A fax submission cannot be processed without the
barcode cover sheet.
Forms using the fax method will be kept for 30 days
to allow a provider to upload the supporting documentation. If the supporting
documentation is not received, the forms will be purged.
Once a TPL form is completed and supporting
documentation is received, it will be used in the claims review process to
determine claims payment or denial. The claims submission for this process is
detailed below.
The next step is to submit an electronic
claim that will be suspended for review.
How can a provider
submit a claim?
You
can continue to submit claims as you do today. If you use a software vendor,
consult with your software vendor prior to submitting claims to ensure they are
populating the proper loops and segments. When submitting claims with a TPL
denial, you include the appropriate primary payer information (most importantly the adjustment
information with corresponding denial reason from the payer) and an ACN
(Attachment Control Number). These items are required for claims to process
correctly and not deny for TPL edits. The ACN must be obtained from the AL Medicaid
Interactive Web Portal by completing the new TPL Attachment form as described
above.
• For claims
submitted through 5010 X12:
1. In
either Loop 2320 (Header) or Loop 2430 (Detail) a CAS segment corresponding to
the Primary Payers Adjustment amount (for these claims it should equal the
billed amount) and denial reason (CARC) must be submitted.
• Example - CAS*OA*59*124.01~
2. In either Loop 2300 (Header)
or Loop 2400 (Detail) a PWK Segment must be submitted with the below values:
• PWK01 = EB
• PWK02 = FT or FX
• PWK05 = AC
PWK06 = Your Provided Attachment Control Number
• Example - PWK*EB*FX***AC*123456789
• For claims submitted on the
Medicaid Interactive Web Portal:
New panels have been
added to the TPL Information Section of the claim forms to allow for submission
of data elements necessary to process these denied claims correctly.
1.
The new supplemental information panel is now
available to add the appropriate ACN to your claim.
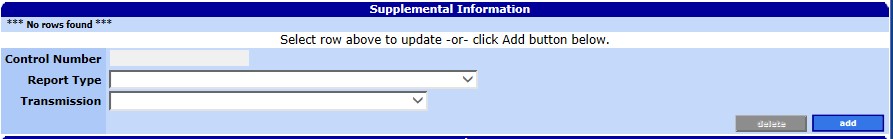
•
By clicking add, the panel will create a record and auto-populate the Report
Type as EB and Transmission type as FT (valid values for the TPL Denial
Process).
•
Populate the Control number field with the
ACN provided by the TPL Attachment form.
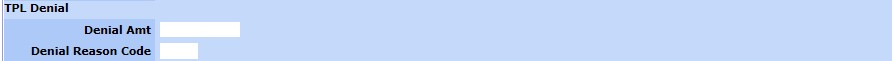
2. The New TPL Denial subpanel is now available to provide the amount
denied by the Primary Insurance and the appropriate denial reason (CARC)
provided by the primary payer.
•
For claims submitted through
PES:
1. PES does not currently allow claims to be submitted with this information, but a software upgrade (3.11) will be
available in the near future.
Medicaid Claim Denials:
If all the required elements for a TPL Denied claim are not correctly
submitted, and/or the information (Dates, Providers, and Recipients) on the
claim does not match that of the corresponding ACN, then appropriate error
responses will be returned.
Some
examples of what a
provider can expect to see
on the denied claim include:
|
2570 TPL DENIAL CAS CODE NOT SUBMITTED
|
|
2572 ATTACHMENT CONTROL NUMBER NOT
SUBMITTED
|
|
2573 ATTACHMENT NUMBER NOT ON FILE
|
|
2574 ATTACHMENT STATUS IS REJECTED
|
|
2575 ATTACHMENT PROVIDER MISMATCH
|
|
2576 ATTACHMENT RECIPIENT MISMATCH
|
|
2577 ATTACHMENT DATE MISMATCH
|
If all the required
elements for a TPL Denied claim are correctly submitted and the information on
the claim matches the documentation which corresponds to the submitted ACN,
then the claim will be suspended for internal review. The claim along with the
supporting documentation will be used to determine if the claim should Pay,
Deny, or if additional documentation is required.
The Current Procedural Terminology (CPT) and Current Dental Terminology
(CDT) codes descriptors, and other data are copyright © 2020
American Medical Association and © 2020 American Dental Association (or such other date publication of CPT and
CDT). All rights reserved. Applicable FARS/DFARS apply.